SAFETY PLAN (BRIEF DESCRIPTION OF THE PLAN CONVEYED TO THE CLIENT
SAFETY PLAN (BRIEF DESCRIPTION OF THE PLAN CONVEYED TO THE CLIENT
PATIENT INFORMATION:
| F20.9 | Schizophrenia, unspecified | |
| Patient Age: | 51 Years |
MaleMedications: Quetiapine fumarate 50mg take 1 tablet by mouth at bedtime for psychosis.
Abilify 5mg take 1 tablet by mouth twice a day for psychosis. (Antipsychotics, 2nd Generation (Atypical)
| SAFETY PLAN (BRIEF DESCRIPTION OF THE PLAN CONVEYED TO THE CLIENT): | VISUAL OBSERVATIONS Q15 MINUTES. REASSURANCE AND EMOTIONAL SUPPORT PROVIDED. TEACHING IN REGARDS MEDICATION COMPLIANCE AND MEDICATION SIDE EFFECTS. THE PATIENT WAS ENCOURAGED TO PARTICIPATE TO GROUP THERAPY. CURRENT TREATMENT AND PLAN WAS PRESENTED AND DISCUSSED WITH THE PATIENT WHO DISPLAYED UNDERSTANDING AND AGREED WITH THE PRESENTED PLAN. THE PATIENT WILL BE REASSESSED ACCORDINGLY. |
___________________________________________________________________________
DEMOGRAPHIC DATA
- Patient’s age and patient’s gender identity
- IT MUST BE HIPAA compliant.
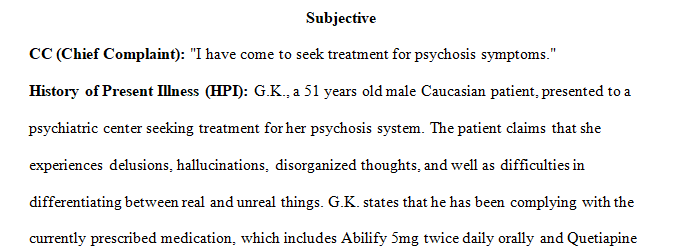
SUBJECTIVE
- Chief Complaint (CC):
- Place the patient’s CC complaint in Quotes
- History of Present Illness (HPI):
- Reason for an appointment today.
- The events that led to hospitalization or clinic visits today.
- Include symptoms, relieving factors, and past compliance or non-compliance with medications
- Any adverse effects from past medication use
- Sleep patterns – number of hours of sleep per day, early wakefulness, inability to initiate sleep, inability to stay asleep, etc.
- Suicide or homicide thoughts present
- Any self-care or Activity of Daily Living (ADL) such as eating, drinking liquids, self-care deficits, or issues noted?
- Presence/description of psychosis (if psychosis, command or non-command)
- Past Psychiatric History (PSH):
- Past psychiatric diagnoses
- Past hospitalizations
- Past psychiatric medications use
- Any non-compliance issues in the past?
- Any meds that didn’t work for this patient?
- Family History of Psychiatric Conditions or Diagnoses:
- Mother/father, siblings, grandparents, or direct relatives
- Social History:
- Include nutrition, exercise, substance use (details of use), sexual history/preference, occupation (type), highest school achievement, financial problems, legal issues, children, and history of personal abuse (including sexual, emotional, or physical).
- Allergies:
- To medications, foods, chemicals, and others.
- Review of Systems (ROS) (Physical Complaints):
- Any physical complaints by the body system? (Respiratory, Cardiac, Renal, etc.)
OBJECTIVE
- Mental Status Exam:
- This is not a physical exam.
- Mental Status Exam (MSE)
ASSESSMENT (DIAGNOSIS)
- Differentials
- Two (2) differential diagnoses with ICD-10 codes.
- Must include rationale using DSM-5 Criteria (Required)
- Why didn’t you pick these as a major diagnosis?
- Working Diagnosis
- Final or working diagnosis (1), with ICD-10 code.
- Must include rationale using DSM-5 criteria required – Which symptoms/signs in the DSM-5 the patient matches mostly)
Plan
- Treatment Plan (Tx Plan):
- Pharmacologic: Include complete information for each medication(s) prescribed
- Refill Provided: Include complete information for each medication(s) refilled
- Patient Education:
- Including specific medication teaching points
- Was the risk versus benefit of the current treatment plan addressed for meds or treatment
- Risk versus benefit of non-FDA approved for working diagnosis – Off-label use of medication education to patient addressed?
- Prognosis:
- Make Decision for prognosis: Good, Fair, Poor
- Provide brief statement lending support for or against the decided prognosis.
- Therapy Recommendations:
- Type(s) of therapy recommended.
- Referral/Follow-up:
- Did you recommend follow-up with a Psychiatrist, PCP, or other specialist or healthcare professionals?
- When is the subsequent follow-up?
- Include the rationale for the F/U recommendation or referral.
Reference(s):
- Include American Psychological Association (APA) formatted references.
- Include a reference from the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Health Disorders (DSM-5) or the accompanying Desk Reference of Diagnostic Criteria from DSM-5.
Rubric
Problem-focused SOAP Note
| Problem-focused SOAP Note | ||
| Criteria | Ratings | Pts |
| This criterion is linked to a Learning OutcomeSubjective | 25 to >20.0 pts Accomplished Subjective data, including the analysis is well organized in a SOAP format, with C/C, Past Psychiatric History, Social History, and other pertinent past and current diagnostic details. SOAP Note is complete, concise, and relevant with no extraneous data. 20 to >15.0 pts Satisfactory Subjective data, including the analysis is well organized in a SOAP format, with C/C, Past Psychiatric History, Social History, and other pertinent past and current diagnostic details. Some extraneous data is present, with one minor data point missing 15 to >14.0 pts Needs Improvement Subjective data, including the analysis is not well organized or presented in a varied format. Required data is missing. Too much extraneous data is present, or 2-3 minor data points are missing. 14 to >0 pts Unsatisfactory Subjective data, including the analysis is inadequate and is not organized. Objective or other data is mixed into the subjective data. Critical data is missing. | 25 pts |
| This criterion is linked to a Learning OutcomeObjective | 25 to >20.0 pts Accomplished Objective information, including the Mental Status Exam MSE) is complete, concise, well-organized, and well-written. Includes pertinent psychiatric information. They are organized by MSE list format. No extraneous information is included. 20 to >15.0 pts Satisfactory Objective information, including the Mental Status Exam (MSE) is partially incomplete, organized, and satisfactorily written. Includes pertinent psychiatric information with additional extraneous data included. Somewhat organized in MSE list format. 15 to >14.0 pts Needs Improvement Objective information, including the Mental Status Exam (MSE) is incomplete and loosely organized, with improvements required. Relevant psychiatric information is omitted. 14 to >0 pts Unsatisfactory Objective information, including the Mental Status Exam is absent or disorganized in presentation, adheres to no specific format, or grossly omits relevant psychiatric information. | 25 pts |
| This criterion is linked to a Learning OutcomeAssessment | 25 to >20.0 pts Accomplished Assessment with differential Dignosis are correct with DSM-5 code(s) and supported by subjective and objective data. Includes: 1 working Dx and 2 Differential Dx. 20 to >15.0 pts Satisfactory Assessment with differential Dignosis are correct with DSM-5 code(s) and supported mainly by subjective and objective data. Missing at least one (1) pertinent subjective ot objective data for the working diagnosis is correct. 15 to >14.0 pts Needs Improvement Diagnosis and/or Differential Dx are correct with DSM-5 code(s) and supported mainly by subjective and objective data. Or differential diagnoses are adequate with an incorrect working diagnosis. 14 to >0 pts Unsatisfactory All diagnoses (working and differential diagnoses) are incorrect or are missing based on the subjective and objective data presented. | 25 pts |
| This criterion is linked to a Learning OutcomePlan | 25 to >20.0 pts Accomplished The plan is well-organized, complete, evidence-based, and patient-centric. It comprehensively addresses each diagnosis and is individualized to the specific patient. 20 to >15.0 pts Satisfactory The plan is organized, complete, evidence-based, and patient-centric. It comprehensively addresses each diagnosis and is individualized to the specific patient. The plan is missing 1-2 of the required items. 15 to >14.0 pts Needs Improvement The plan is less organized and is not based on evidence. Fails to address each diagnosis sufficiently or is not individualized or patient-centric The plan is missing more than 2 of the required items. 14 to >0 pts Unsatisfactory The plan is disorganized, absent, or missing all the required items. | 25 pts |
Requirements: 4 pages
Nursing
Answer preview for the paper on ‘SAFETY PLAN (BRIEF DESCRIPTION OF THE PLAN CONVEYED TO THE CLIENT’
APA 1096 words
Click the purchase button below to download full answer…….
