Patient initial (one initial only), age, and gender must be Health Insurance Portability and Accountability
Patient initial (one initial only), age, and gender must be Health Insurance Portability and Accountability
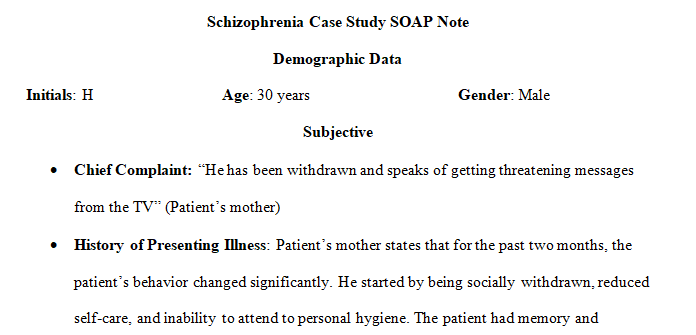
Demographic Data
- Patient initial (one initial only), age, and gender must be Health Insurance Portability and Accountability (HIPPA) compliant.
Subjective
- Chief Complaint (CC)
- History of Present Illness (HPI) (symptoms) in paragraph format
- Past Medical History (PMH): Current problem-focused and document pertinent information only.
- Current Medications:
- Medication Allergies:
- Social History: For current problem-focused and document only pertinent information only.
- Family History: For current problem-focused and document only pertinent information only.
- Review of Systems (ROS) as appropriate:
Objective
- Vital signs
- Mental Status Exam
- Physical findings listed by body systems, not paragraph form.
- Patient Health Questionnaires, Screenings, and the results (PHQ-9, GAD 7, suicidal)
Assessment (Diagnosis/ICD10 Code)
- Include all diagnoses that apply to this visit.
- Include one differential diagnosis.
Plan
- Dx Plan (lab, x-ray)
- Tx Plan: (meds)
- Pt. Education, including specific medication teaching points.
- Safety Plan
- Referral/Follow-up
| Mini SOAP Note | ||
| Criteria | Ratings | Pts |
| This criterion is linked to a Learning OutcomeSubjective | 15 to >12.0 ptsAccomplishedSOAP format is well organized, with C/C, History of present Illness, past medical history, Medications, Allergies, Social Hx, family history, and other pertinent past and current diagnostic details. SOAP Note is complete, concise, and relevant with no extraneous data 12 to >10.0 ptsSatisfactorySOAP format is well organized, with C/C, History of present Illness, past medical history, Medications, Allergies, Social Hx, Family history, and other pertinent past and current diagnostic details. Some extraneous data is present, with one minor data point missing. 10 to >5.0 ptsNeeds ImprovementSOAP format analysis is not well organized or presented in a varied format. Required data is missing. Too much extraneous data is present, or 2-3 data points are missing 5 to >0 ptsUnsatisfactorySymptom analysis is inadequate and is not organized. Objective or other data is mixed into the subjective data. Critical data is missing | 15 pts |
| This criterion is linked to a Learning OutcomeObjective | 15 to >12.0 ptsAccomplishedThe Mental Status Exam is complete, concise, well-organized, and well-written. Includes pertinent psychiatric information. Organized by MSE list format. No extraneous information is included. 12 to >10.0 ptsSatisfactoryThe Mental Status Exam is partially incomplete, organized, and satisfactorily written. Includes pertinent psychiatric information with additional extraneous details included. Somewhat organized in MSE list format. 10 to >5.0 ptsNeeds ImprovementThe Mental Status Exam is incomplete and loosely organized, with improvements required. Therefore, relevant psychiatric information is omitted. 5 to >0 ptsUnsatisfactoryMental Status Exam is absent, disorganized in presentation, adheres to no specific format, or grossly omits relevant or pertinent psychiatric information. | 15 pts |
| This criterion is linked to a Learning OutcomeAssessment | 15 to >12.0 ptsAccomplishedDiagnosis and Differential Dx are correct with DSM-5 code(s) and supported by subjective and objective data. Includes: 1 working Dx and 1 Differential Dx. 12 to >10.0 ptsSatisfactoryDiagnosis and Differential Dx are correct with DSM-5 code(s) and supported mainly by subjective and objective data. One pertinent differential diagnosis is not listed according to subjective and objective data. However, the working diagnosis is correct. 10 to >5.0 ptsNeeds ImprovementDiagnosis and Differential Dx are correct with DSM-5 code(s) and supported mainly by subjective and objective data. Missing pertinent differential diagnoses based on subjective and objective data presented. Or differential diagnoses are adequate with an incorrect working diagnosis. 5 to >0 ptsUnsatisfactoryAll diagnoses (working and differential diagnoses) are incorrect or missing based on the subjective and objective data presented | 15 pts |
| This criterion is linked to a Learning OutcomePlan | 15 to >12.0 ptsAccomplishedThe plan is well-organized, complete, evidence-based, and patient-centric. It comprehensively addresses the diagnosis and is individualized to the specific patient. *Plan requirements: prescribed medications, if any; explanation of off-label medication use, if prescribed; risks and benefits of medicines identified; therapy recommendations; patient education; referral/follow-up; and health maintenance. 12 to >10.0 ptsSatisfactoryThe plan is organized, complete, evidence-based, and patient-centric. It comprehensively addresses the diagnosis and is individualized to the specific patient. The plan is missing one of the required items. 10 to >5.0 ptsNeeds ImprovementThe plan is less organized and is not based on evidence. Fails to address each diagnosis sufficiently or is not individualized or patient-centric The plan is missing two or more of the required items. 5 to >0 ptsUnsatisfactoryThe plan is disorganized, absent, or missing all the required items. | 15 pts |
- Patient :
- Schizophrenia, unspecified
- 30 Years
- Male
- medications: Haldol 10mg take 1 tablet by mouth twice a day for psychosis.
Cogentin 0.5mg take 1 tablet by mouth twice a day for involuntary movements.
Requirements: 1-2 page
Nursing
Answer preview for the paper on ‘Patient initial (one initial only), age, and gender must be Health Insurance Portability and Accountability’
APA 746 words
Click the purchase button below to download full answer…….
