Select a child/adolescent or adult patient from your clinical experience that presents with a significant concern
Select a child/adolescent or adult patient from your clinical experience that presents with a significant concern
COMPLEX CASE STUDY PRESENTATION
In Weeks 4, 7, and 9 of the course, you will participate in clinical discussions called grand rounds. In one of these three weeks, you will be a presenter as well as help facilitate the online discussion; in the others you will be an active discussion participant. When it is your week to present, you will create a Focused SOAP note and a short didactic (teaching) video presenting a real (but de-identified) complex patient case from your practicum experience.
You should have received an assignment from your Instructor letting you know which week of the course you are assigned to present.
RESOURCES
Be sure to review the Learning Resources before completing this activity.
Click the weekly resources link to access the resources.
TO PREPARE:
- Review this week’s Learning Resources and consider the insights they provide. Also review the Kaltura Media Uploader resource in the left-hand navigation of the classroom for help creating your self-recorded Kaltura video.
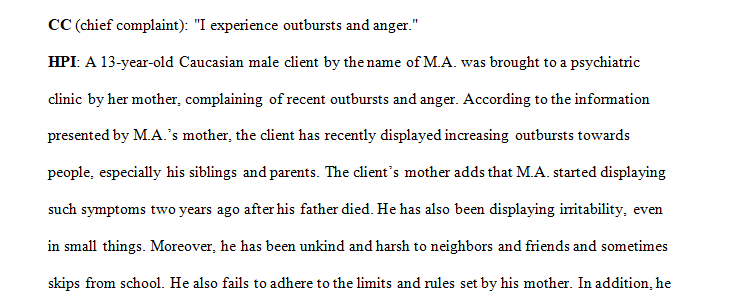
- Select a child/adolescent or adult patient from your clinical experience that presents with a significant concern. ( Patient case: Chief complaint: HPI: Patient M. A is a 13-year-old Caucasian male whopresents today with her mother for a follow-up visit. Mother reports recentoutbursts and anger towards her and pt siblings. The patient father died twoyears ago from lung cancer, and the patient became increasingly irritable.The mother states they sought help, and pt was diagnosed with depression andparticipated in therapy. Pt verbalized his sleep has improved. The pt hasbeen harsh and unkind to his friends and neighbors and most often will skipschool. Pt refuses to follow most rules and limits set up by his mother.Mental Status Examination: Patient is alert and oriented t person, place, andtime. He appears irritable, angry, and uncooperative with his mother and
practitioner. Pt. speech is clear and loud. He denies self-harm and suicideintent. Pt has unkempt hair but is groomed appropriately for the weather. Histhought process is organized, and memory is intact for recent and remoteevents. Deny hallucinations and no delusional thought or ideas noted.Diagnosis: F91.3 Oppositional Defiant Disorders F33.0 major depressivedisorder. Treatment plan Pharmacological: Continue with Zoloft 25mg PO dailyAdderall 5mg PO increased to 10 mg PO daily Non-Pharmacological: The patientwill continue with therapy. The risk, benefits, and potential adverse effectsof medications discussed with the patient and mother and verbalizeunderstanding. Follow up scheduled in 2 weeks.) - Create a focused SOAP note for this patient using the template in the Resources. All SOAP notes must be signed by your Preceptor. When you submit your SOAP note, you should include the complete SOAP note as a Word document and PDF/images of completed assignment signed by your Preceptor. You must submit your SOAP Note using Turnitin.
Please Note: Electronic signatures are not accepted. If both files are not received by the due date, Faculty will deduct points per the Walden Late Policies. - Then, based on your SOAP note of this patient, develop a video case study presentation. Take time to practice what you will say beforehand, and ensure that you have the appropriate lighting and equipment to record the presentation.
- Your presentation should include objectives for your audience, at least 3 possible discussion questions/prompts for your classmates to respond to, and at least 5 scholarly resources to support your diagnostic reasoning and treatment plan.
Video assignment for this week’s presenters:
Record yourself presenting the complex case study for your clinical patient. In your presentation:
- Dress professionally and present yourself in a professional manner.
- Display your photo ID at the start of the video when you introduce yourself.
- Ensure that you do not include any information that violates the principles of HIPAA (i.e., don’t use the patient’s name or any other identifying information).
- State 3–4 objectives for the presentation that are targeted, clear, use appropriate verbs from Bloom’s taxonomy, and address what the audience will know or be able to do after viewing.
- Present the full complex case study. Include chief complaint; history of present illness; any pertinent past psychiatric, substance use, medical, social, family history; most recent mental status exam; current psychiatric diagnosis including differentials that were ruled out; and plan for treatment and management.
- Report normal diagnostic results as the name of the test and “normal” (rather than specific value). Abnormal results should be reported as a specific value.
- Pose three questions or discussion prompts, based on your presentation, that your colleagues can respond to after viewing your video.
- Be succinct in your presentation, and do not exceed 8 minutes. Specifically address the following for the patient, using your SOAP note as a guide.
- Subjective: What details did the patient provide regarding their chief complaint and symptomology to derive your differential diagnosis? What is the duration and severity of their symptoms? How are their symptoms impacting their functioning in life?
- Objective: What observations did you make during the psychiatric assessment?
- Assessment: Discuss their mental status examination results. What were your differential diagnoses? Provide a minimum of three possible diagnoses and why you chose them. List them from highest priority to lowest priority. What was your primary diagnosis, and why? Describe how your primary diagnosis aligns with DSM-5-TR diagnostic criteria and is supported by the patient’s symptoms.
- Plan: What was your plan for psychotherapy (include one health promotion activity and patient education)? What was your plan for treatment and management, including alternative therapies? Include pharmacologic and nonpharmacologic treatments, alternative therapies, and follow-up parameters, as well as a rationale for this treatment and management plan. Discuss an identified social determinate of health impacting this patient’s mental health status and provide your recommendation for a referral to assist this patient in meeting this identified need (students will need to conduct research on this topic both in the literature and for community resources).
- Reflection notes: What would you do differently with this patient if you could conduct the session again? If you are able to follow up with your patient, explain whether these interventions were successful and why or why not. If you were not able to conduct a follow-up, discuss what your next intervention would be.
see samples attached.
You do not have to do the recordings, however also create a written portion for the the recording. let me know is you have questions
Requirements: use template
Answer preview for the paper on ‘Select a child/adolescent or adult patient from your clinical experience that presents with a significant concern’
APA 1597 words
Click the purchase button below to download full answer…….
